

 Back to Latest News
Back to Latest News
Authors: Kosalaraksa; Mehlsen; Vesikari; Forstén; Helm; Van Damme; Joura; Ciprero; Maansson; Luxembourg; Sobanjo-ter Meulen
Summary
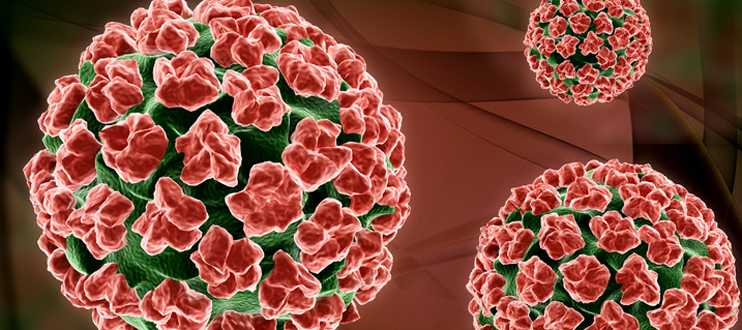
In 1995 the International Agency for Research on Cancer classified HPV16/18 as cervical carcinogens, and in 2011, the group was expanded to include HPV31/33/35/39/45/51/52/56/58/59. After HPV16/18, HPV31/33/35/45/52/58 are the most frequent types detected in invasive cervical cancer worldwide. Several previous studies have estimated the prevalence of HPV16/18/31/33/45/52/58 in invasive cervical cancer and pre-cancers to be approximately 90%, with good consistency across regions. A second generation 9-valent HPV (9vHPV) vaccine has been developed which contains these seven high-risk types, in addition to HPV6/11. The vaccine has been shown to be safe and highly efficacious against infection and disease related to these types.
A booster dose of diphtheria, tetanus, acellular pertussis, and inactivated poliovirus vaccines is recommended for adolescents. Licensed HPV vaccines have been introduced in the national vaccination programs of more than 40 countries. Although the age range of the primary target age group varies by country, all of these programs target young adolescents.
Non-inferiority of anti-HPV GMTs and seroconversion rates for all 9vHPV antigens were demonstrated for the concomitant group compared with the non-concomitant group. Seroconversion rates for the 9vHPV vaccine types were 99.8% in both groups at month 7. For REPEVAX (Tdap-IPV vaccine), noninferiority of immune response was established for diphtheria, tetanus, and all polio and pertussis antigens for both groups. There were no vaccine-related serious AEs.
Overall, concomitant administration of 9vHPV vaccine and REPEVAX was generally well tolerated and did not interfere with the immune response to either vaccine. This strategy would minimize the number of visits required to deliver each vaccine individually.
Go to the article.