

 Back to Latest News
Back to Latest News
Here's WAidid first reading suggestion tackling the urgent issue of 2019-nCoV. It titles Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China and was published at the beginning of February on JAMA.
SUMMARY:
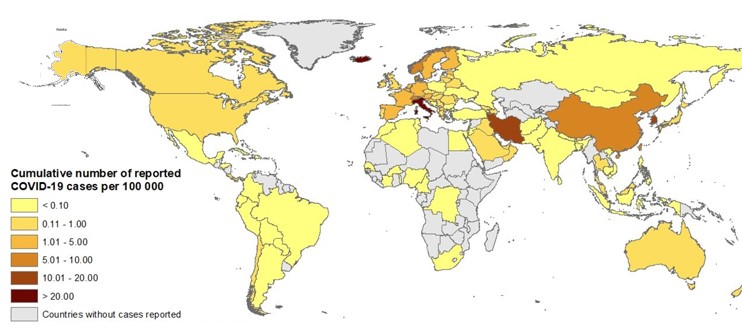
In December 2019, a cluster of acute respiratory illness, now known as novel coronavirus–infected pneumonia (NCIP), occurred in Wuhan (China). The disease has rapidly spread to other areas. As of January 31, 2020, a total of 9692 NCIP cases in China have been confirmed. Internationally, cases have been reported in 24 countries and 5 continents. Full-genome sequencing and phylogenic analysis indicated that 2019-nCoV is a distinct clade from the betacoronaviruses associated with human severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). While the origin of the 2019-nCoV is still being investigated, current evidence suggests spread to humans occurred via transmission from wild animals. Patients’ clinical manifestations included fever, nonproductive cough, dyspnea, myalgia, fatigue, normal or decreased leukocyte counts, and radiographic evidence of pneumonia. Organ dysfunction and death can occur in severe cases. Case reports confirmed human-to-human transmission of NCIP. At present, there are no effective therapies or vaccines for NCIP.
The authors reported the clinical characteristics of 138 hospitalized patients with NCIP.
All consecutive patients with confirmed NCIP admitted to Zhongnan Hospital of Wuhan University, from January 1 to January 28, 2020, were enrolled. The clinical outcomes were monitored up to February 3, 2020, the final date of follow-up.
Throat swab samples were collected for extracting 2019-nCoV RNA.
The median age was 56 years old. Of these patients, 102 (73.9%) were admitted to isolation wards, and 36 (26.1%) were admitted and transferred to the ICU, because of the development of organ dysfunction. 64 patients (46.4%) had 1 or more coexisting medical conditions.
The most common symptoms, at onset of illness, were fever (98.6%), fatigue (69.6%), dry cough (59.4%), myalgia (34.8%), and dyspnea (31.2%).
Compared with patients who did not receive ICU care (n = 102), patients who required ICU care (n = 36) were significantly older (P < .001) and were more likely to have underlying comorbidities.
Heart rate, respiratory rate, and mean arterial pressure did not differ between patients who received ICU care and patients who did not receive ICU care.
As of February 3, 2020, 85 patients (61.6%) were still hospitalized. A total of 47 patients (34.1%) had been discharged, and 6 patients (4.3%) had died. Of the 36 patients admitted to the ICU, 11 were still in the ICU, 9 had been discharged to home, 10 had been transferred to the general wards, and 6 had died. Of the 11 patients who remained in the ICU, 6 received invasive ventilation. Common complications among the 138 patients included shock, ARDS, arrhythmia, and acute cardiac injury. Patients who received care in the ICU were more likely to have one of these complications than non-ICU patients.
Most patients received antiviral therapy, and many received antibacterial therapy. In the ICU, 4 patients received high-flow oxygen, 15 received noninvasive ventilation, and 17 invasive mechanical ventilation.
During hospitalization, most patients had marked lymphopenia; non-survivors developed more severe lymphopenia, higher white blood cell counts and neutrophil counts, and higher D-dimer level than those in survivors.
Of the 138 patients, 57 (41.3%) were presumed to have been infected in hospital.
The authors underlined that this represents the largest case series to date of hospitalized patients with NCIP, and that their data suggest rapid person-to-person transmission of 2019-nCoV, and that age and comorbidity may be risk factors for poor outcome. Moreover, they highlighted that the laboratory abnormalities suggest that 2019-nCoV infection may be associated with cellular immune deficiency, coagulation activation, myocardia injury, hepatic injury, and kidney injury, which are similar to those previously observed in patients with MERS-CoV and SARS-CoV infection. They warned that, as no specific treatment is currently available, the approach to this disease is to control the source of infection, use of personal protection precaution to reduce the risk of transmission, and early diagnosis, isolation, and supportive treatments for affected patients.
AUTHORS: Dawei Wang, MDBo Hu, MDChang Hu, MD; et al.
You can read the full article here.