

 Back to Suggested Publications
Back to Suggested Publications
The reading WAidid suggests this week is a recent article published on NEJM, Benefits and Risks of Antiretroviral Therapy for Perinatal HIV Prevention. The article reports a trial called PROMISE (Promoting Maternal and Infant Survival Everywhere),which compares benefits and risks of various antiretroviral strategies for the prevention of mother-to-child transmission oh HIV.
SUMMARY:
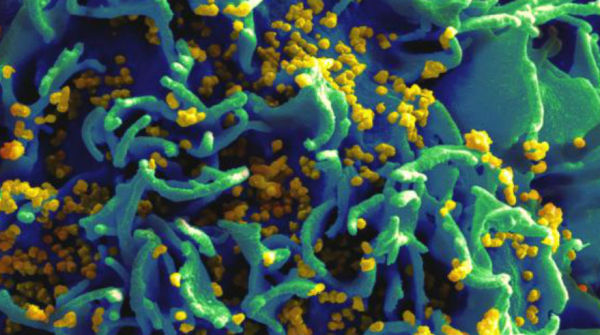
Antiretroviral regimens used for the prevention of mother-to-child transmission of the human immunodeficiency virus (HIV) have evolved from the first successful trial, that used zidovudine single-drug prophylaxis in 1994, to current triple-drug regimens. Although there are clear benefits of combination antiretroviral therapy (ART), for mothers and infants, these do not come without risks. The Promoting Maternal and Infant Survival Everywhere (PROMISE) trial compared the relative efficacy and safety of various proven antiretroviral strategies for the prevention of mother-to-child transmission, during pregnancy, among asymptomatic HIV-infected women, with high CD4 counts. The authors presented the results of this study.
The PROMISE trial, conducted at 14 sites in seven countries, compared open-label strategies and included sequential randomizations: antepartum randomization to one of three regimens, and postpartum randomization.
In the antepartum component, women were randomly assigned to one of three regimens: zidovudine plus intrapartum single-dose nevirapine with 6 to 14 days of tenofovir and emtricitabine post partum (zidovudine alone); zidovudine, lamivudine, and lopinavir–ritonavir (zidovudine-based ART); or tenofovir, emtricitabine, and lopinavir–ritonavir (tenofovir-based ART). All regimens were continued through 6 to 14 days post partum. All infants received nevirapine from birth until postpartum randomization.
From April 2011 to September 2014, 3529 mother–infant sets were enrolled. 39 women were excluded. Of the 3490 mother–infant sets included in analyses, there were 3202 live births. Most women were African, young, and asymptomatic. At screening, the median CD4 count was 530 cells per cubic millimeter, and 3% of the women were HBsAg-positive. The rate of trial-drug discontinuation was low.
All three regimens studied had a HIV-transmission rate of less than 2%, but the ART regimens had significantly lower rates of transmission than zidovudine alone. However, both ART regimens were associated with higher rates of adverse events (P = 0.008 for zidovudine-based ART) and higher abnormal chemical values (P < 0.001 and P = 0.03, for zidovudine-based ART and tenofovir-based ART, respectively) than zidovudine alone; no significant difference between the two ART regimens was observed.
Higher rates of adverse pregnancy outcomes were observed with zidovudine-based ART and tenofovir-based ART, than with zidovudine alone, but no significant difference between the two ART regimens was observed. However, women receiving tenofovir-based ART had significantly higher rates than those receiving zidovudine-based ART of severe adverse pregnancy outcomes (P = 0.02) and very preterm delivery (P = 0.04).
Among 3202 live births, no significant differences were observed among the groups regarding adverse outcomes other than death. No significant difference in infant deaths was observed between the group assigned to zidovudine-based ART and the zidovudine-alone group; the same was observed between the tenofovir-based ART group and the zidovudine-alone group, but the group assigned to tenofovir-based ART had significantly more infant deaths than the group assigned to zidovudine-based ART (P<0.001).
The authors concluded that the PROMISE trial showed superior efficacy of triple-drug ART, as compared with zidovudine plus single-dose nevirapine, for the prevention of mother-to-child transmission in HIV-infected women with high CD4 cell counts, but it also showed higher rates of adverse events. The authors highlighted that the most efficacious and safest triple-drug ART regimens during pregnancy remain to be defined, emphasizing the need for continued research.
AUTHORS:
Mary G. Fowler, Min Qin, Susan A. Fiscus, Judith S. Currier, Patricia M. Flynn, Tsungai Chipato, James McIntyre, Devasena Gnanashanmugam, George K. Siberry, Anne S. Coletti, Taha E. Taha, Karin L. Klingman, Francis E. Martinson, Maxensia Owor, Avy Violari, Dhayendre Moodley, Gerhard B. Theron, Ramesh Bhosale, Raziya Bobat, Benjamin H. Chi, Renate Strehlau, Pendo Mlay, Amy J. Loftis, Renee Browning, Terence Fenton, Lynette Purdue, Michael Basar, David E. Shapiro, and Lynne M. Mofenson