

 Back to Suggested Publications
Back to Suggested Publications
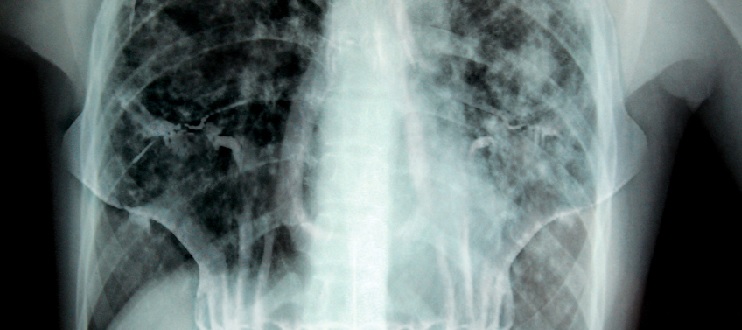
Guidelines for treatment of drug-susceptible tuberculosis and patient care (2017 update)
The update of the Guidelines for treatment of drug-susceptible tuberculosis and patient care is important in the context of the End TB Strategy, which recommends treatment and patient support for all people with TB. This update by WHO aims to use the best available evidence on the treatment of drug-susceptible TB and interventions to ensure adequate patient care and support in order to inform policy decisions made in these technical areas by national TB control programme managers, national policy-makers and medical practitioners in a variety of geographical, economic and social settings.
The objectives of the updated Guidelines for treatment of drug-susceptible tuberculosis and patient care are:
1) to provide updated recommendations based on newly emerged evidence on the treatment of drug-susceptible TB and patient care; and
2) to provide a summary of changes in the new guidelines together with all the existing and valid WHO recommendations on the treatment of drug-susceptible TB and TB patient care.
The main highlights of the guidelines are:
The article is available here.