

 Back to Suggested Publications
Back to Suggested Publications
The article we suggest today, "Guillain–Barré syndrome", recently published on Autoimmunity Reviews, focuses on GBS, the available therapies and the future perspectives of research in this field.
SUMMARY:
Guillain–Barré syndrome (GBS) is the most frequent cause of acute paralytic neuropathy. The exact cause of GBS is unknown, but 50–70% of cases appear 1–2 weeks after a respiratory or gastrointestinal infection, or another immune stimulus. The interplay between the microbial and host factors is still unclear, and nothing is known about the genetic and environmental factors, that affect an individual's susceptibility to the disease. This review summarizes the clinical features and diagnostic criteria of GBS, and proposes an algorithm for its management.
GBS has a reported annual incidence of 0.5–2 cases per 100,000 people. Although many different infections have been identified in patients with GBS, case–control studies have revealed associations with only a few pathogens: Campylobacter jejuni, cytomegalovirus, Epstein–Barr virus, measles, influenza A virus and Mycoplasma pneumoniae, enterovirus D68, and, more recently, Zika virus. Although some authors have reported GBS associated to some vaccines (rabies and influenza A virus), there is little evidence to support a causal association with most vaccines.
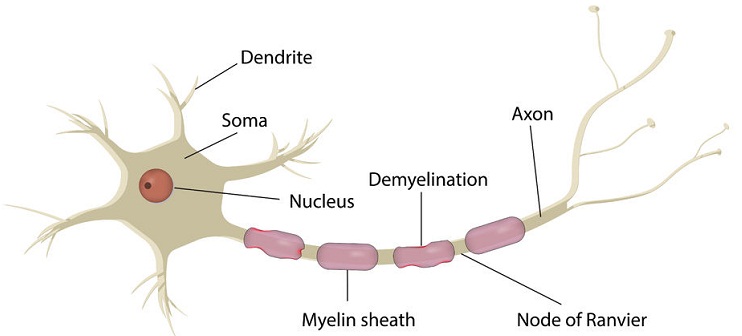
GBS occurs in healthy people, and is not typically associated with an autoimmune or other systemic disorder; it is mainly humoral mediated. An interesting mechanism, that could have a role in GBS, is represented by the T cell epitope redundancy, which might be the link between pathogens and autoimmune disease.
GBS contains a spectrum of acute idiopathic, usually monophasic, peripheral neuropathies. The symptoms at the time of onset of classic GBS are: pain, paresthesia, numbness, and rapidly progressive bilateral limb weakness. The weakness usually starts in the distal lower extremities and progresses upwards. In addition, patients may present sensory signs, ataxia, and autonomic dysfunction. 20–30% of patients develop complications. GBS is a life-threatening disease with a mortality rate of 3–7%, and those who survive are quite frequently affected by sequelae.
GBS can be difficult to diagnose in young children, because they present their complaints atypically, and a neurological examination is more challenging.
Some diagnostic test could help the diagnosis of GBS: lumbar puncture (cerebrospinal fluid typically shows cyto-albuminological dissociation), nerve conduction studies (abnormalities are most pronounced two weeks after the weakness starts), neuroimaging, and anti-ganglioside antibodies (which can be identified in about 50% of patients).
The treatment of GBS requires a multidisciplinary approach.
The authors concluded that, about one century after it was first described, new information concerning the etiopathogenesis of GBS has allowed the development of new treatment strategies (intravenous immunoglobulin, plasma exchange, interferon-β, steroids, cyclophosphamide, humanized monoclonal antibodies); however, the available therapies are not sufficient in many patients. In order to improve patient outcomes, research should continue to identify new biomarkers of disease severity.
AUTHORS: S. Esposito, M. R. Longo
Here is the link to the full article.